What Really Determines Eye Color? Melanin, Light Scattering & the Science Behind FLAAK Eye Color Change
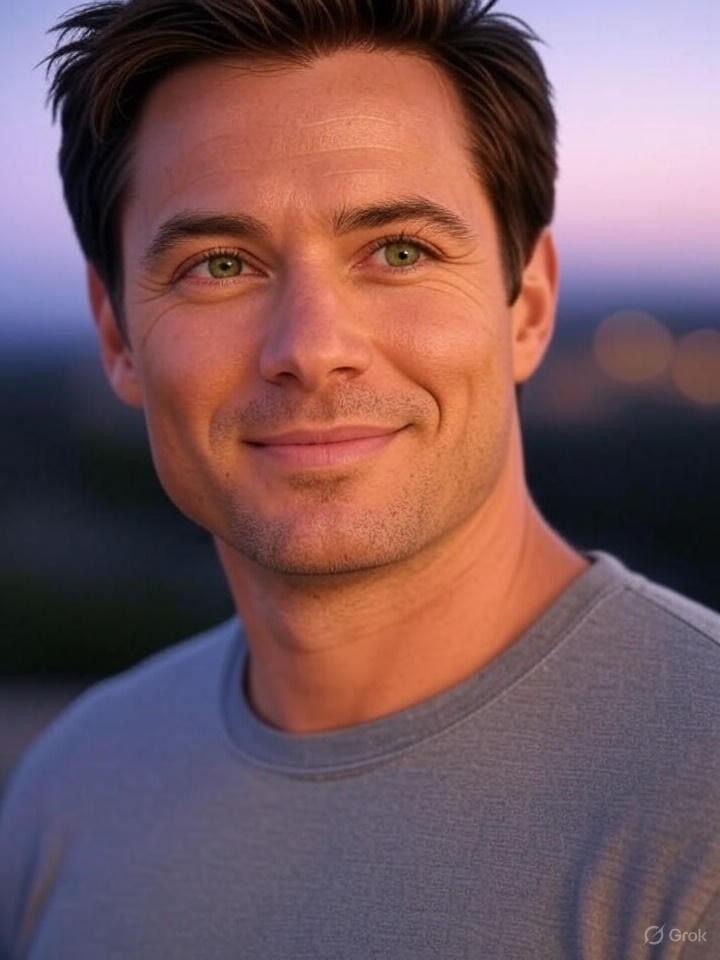
What Really Determines Eye Color? Melanin, Light Scattering & the Science Behind FLAAK Eye Color Change 🧬 What Determines Eye Color? The Biology of Melanin, Light Scattering and the Science Behind FLAAK Eye color is far more complex than simply categorizing it as blue, green, hazel, or brown. It is determined by a combination of melanin concentration, light scattering, and the structural properties of the iris. Modern eye color change procedures such as FLAAK (Keratopigmentation) are built upon these scientific principles. 🔬 1. Melanin: The Primary Factor Shaping Eye Color Melanin in the anterior layer of the iris determines the basic color: High melanin → dark brown Medium melanin → hazel / light brown Low melanin → green Very low melanin → blue Melanin not only adds pigment but also influences how light behaves inside the eye. 🔭 2. Blue Eyes Aren’t Actually Blue — It’s Physics People with blue eyes do not have blue pigment. The iris contains very little melanin, allowing light to pass through and scatter. This process is called Rayleigh scattering, the same phenomenon that makes the sky appear blue. Thus: Blue → minimal pigment + strong light scattering Green → moderate pigment + scattering Hazel → pigment + warm scattering mix This explains why FLAAK pigments look natural—they work with existing optical physics. 🧪 3. Genetics & Epigenetics: Why Eye Color Can Change Eye color is not fixed for life. It may change due to: Infant melanin development Age-related pigment reduction Trauma Hormonal factors This shows that iris pigmentation has natural variability. 🏥 4. How FLAAK Works Scientifically FLAAK places biocompatible pigment inside stromal channels created by femtosecond laser within the cornea. Because the pigment is placed in the cornea—not the iris: No entry into the eye No effect on internal structures Visual acuity remains unchanged The final color appears natural due to internal light diffusion 🌈 5. Why FLAAK Colors Look Natural Pigments diffuse inside stromal tissue, not on the surface. This creates: A soft, natural tone A blend with the patient’s underlying melanin A unique final shade for each person The result is not a “lens look” but a naturally integrated eye color. 📌 Conclusion Eye color is determined by melanin levels and how light interacts with the iris. FLAAK eye color change enhances this natural system safely by modifying corneal light behavior—without touching the iris. This makes FLAAK: Safe Permanent Natural-looking Optically harmonious Meta Description: Eye color is determined by melanin and light scattering. FLAAK eye color change works safely by modifying corneal light behavior without touching the iris. Keywords: eye color science, iris pigmentation, melanin, how eye color is formed, FLAAK eye color change, keratopigmentation, natural-looking eye color change, blue eye genetics Son Güncelleme 18 November 2025 Saat 09:41 am